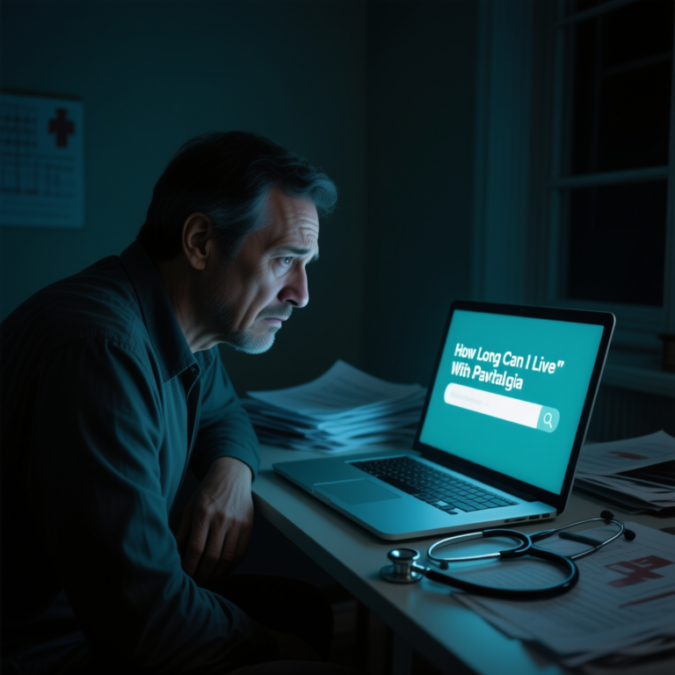
When a person is confronted with a diagnosis of a novel medical condition, it’s natural for one’s mind to spin with questions and concerns, and to become fearful of the unknown. One of the first concerns is, “How long can I live with this?” If you’ve been searching for the phrase, “How long can I live with pavatalgia,” then this article is for you. However, it is imperative to start with the following: Pain is not a recognized medical condition. This is not a term in textbooks, published literature, or the stipulated disease classifications such as ICD-10 or ICD-11.
This means, to answer the question, ‘How long can I live with pavatalgia’ is in fact not answerable because life expectancy is not a concept here, as pavatalgia is not a disease and thus poses no threat to one’s life. This is a feeling of anxiety and concern, most certainly, and it is also most certainly the result of a misconception, a typo, or just some unsubstantiated material sourced from the internet. This article will dissect the term, show you what it may be confused with, and steer you in the right direction so you obtain an accurate diagnosis accompanied by an understanding of what your prognosis truly is.

Examining the Components of the Word Pavatalgia
To understand why the term pavatalgia is not a legitimate diagnosis is to understand the root components of the word pavatalgia using Latin and Greek during the formation of words in the medical field
Pava: That segment of the word has not been defined in the field of medicine. Pavatalgia has no connections to any organ system, no functions, and no pathological processes. It is a misplaced or miswritten medical term.
-Algia is a suffix that is definable, and it means “pain.” This is a suffix that we find in many medical terms like, “neuralgia the pain of the nerve, arthralgia, ” the pain of the joint, and myalgia, ” the pain of the muscle.”
Thus, it can be deduced that the word pavatalgia can only mean pain, and that is the pav. The term pavatalgia means nothing in the medical field. This point is worth dwelling on. The term is a dead end, and pava has no definition. The greater challenge is to identify the medical condition causing the described symptoms.
Is there any word that is pain that is confused with?
The best answer is that pavatalgia is a word that has been misspelled or misused in a medical context. The most probable is Peripheral Artery Disease, also known as PAD or simply Neuralgia.
Peripheral Artery Disease (PAD)
This is most likely the case. As the name of the disorder is sometimes incorrectly received and recorded as “pava peripheral” and/or “pava”. PAD is one of the most common circulatory system problems. Narrowed arteries reduce blood flow to the extremities, most often the legs.
Symptoms. The most common PAD symptom is walking to the point of Claudication. The leg pain and cramping one feels in the calves, thighs, and/or buttocks are triggered by activity and ultimately resolve with rest. This symptom is often ignored because of its similarity to leg pains (which also supports the suffix).
Prognosis and Life Expectancy (the honest answer). Here, we fulfill the ordinary and we face the source of your phobia with a valid condition. PAD is not an immediate threat to your life; however, it is a strong indicator of systemic atherosclerosis. This is also not an immediate threat to your life; systemic atherosclerosis has a substantial impact on the arteries that supply blood to your coronary arteries and brain (the carotid arteries). In that case, although this leg pain is the only leg symptom, it is also a symptom of a higher chain of cardiovascular events that are associated with PAD. Becoming precious. (MACE).
Individuals with PAD likely have a lower life expectancy due to the accompanying risk of cardiovascular comorbidities. Studies indicate that the five-year mortality rate for patients with PAD can be as high as 30% due to cardiovascular events such as myocardial infarction and cerebrovascular accidents.
However, while concerning, this is not a death sentence. Life expectancy will differ, and will often be determined by the severity of the disease, the presence of comorbidities (smoking, diabetes, hypertension, and hyperlipidemia), and, most importantly, treatment. PAD and the risk of life-threatening comorbidities can be so positively altered by aggressive management of the risk factors, and by making lifestyle and behavioral changes such as smoking cessation and physical activity, that not only is the quality of life increased, but PAD can be substantially slowed.
Neuralgia
This is another strong possibility, as the name “Neuralgia” is often misheard and is commonly used to describe nerve pain.
Symptoms: It is characterized by a pain that is posited to be along a nerve that is damaged or irritated and that presents as a “shock-like” symptomatology or burning or tingling and can be present in any region of the body; for instance, “trigeminal” is a neuralgia of the face or “sciatica” is Neuralgia of the leg.
Prognosis and Life Expectancy: Neuralgia and its symptoms arise from other conditions and are not a condition in themselves. Thus, its prognosis symptomatically aligns with the source of the nerve irritation. Etiologies can include a pinched nerve, shingles, diabetes, and even multiple sclerosis.
Neuralgia also does not lead to a shortened prognosis directly, but the pain related to it can be bad enough to affect the overall quality of life significantly. Most of the time, life is not ultimately shortened, though. Indirectly, yes.
The root cause of the Neuralgia truly is and can be life-threatening. Take diabetic neuropathy, to which you would have to manage diabetes carefully, an otherwise uncontrolled aspect that holds numerous other deadly complications. The most important thing to recognize is finding and addressing the root cause to bring the prognosis within the opportunity of a best-case scenario.
The Critical Path Forward: From Fear to Clarity
Since “pavatalgia” does not exist, your entire energy can now shift from searching for its prognosis to a correct diagnosis, which is an exhausting search in itself.
Consult a Medical Professional: This is the most important step by far. Self-diagnosing based on some pretty vague and very concerning criteria that do not even exist is not only dangerous to your mental state, but disheartening as it only serves to fuel your anxiety. An appointment with your primary care physician is best.
How Should You Prepare for the Appointment?
Be as detailed as possible when explaining symptoms. Rather than using “pavatalgia,” say which area hurts, the type of pain (for instance, is it burning, dull, sharp, aching?), the frequency of the pain, duration of the pain, and what causes it to improve or worsen.
Don’t hesitate to share your point of view, for example, “I found the word pavatalgia when searching online, and while it appears to be a medical condition, it’s been proven to be fake. I’m worried about the possible underlying medical condition my pain stems from.” It proves you’ve conducted a productive exploration and are keen to gain more insight.
Diagnostic Testing: is indicative of the symptoms experienced, your physician will conduct a physical examination and may suggest other Testing. An Ankle-Brachial Index (ABI) test is often the first step if there’s a suspicion of PAD. If a nerve problem is suspected, pain in the neck, or an MRI is needed.
Ending accepted: It is Your Legal Right to leave a Situation if You Feel as if Your Medical Provider is Not Keeping Your Interests.
I understand the reasoning behind “how long can I live with pavatalgia?” Unfortunately, there is no consensus in medicine on the cause of pavatalgia. It is nonexistent; it has nothing, including a quality or a life expectancy, because it is not a real disease.
Your fear is also legitimate. The only way to get out of this uncertainty is to get off the futile search for this phantom condition and work with a healthcare professional to uncover the actual source of pain. Peripheral Artery Disease, some form of Neuralgia, or another condition entirely, a valid diagnosis is the first and most necessary step in the process. A correct diagnosis is the only way you and your doctor can outline an effective management plan, control the symptoms, comprehend the genuine long-term prognosis, and ultimately, regain hope for the future and control of your life. The shift in focus should come from “How long do I have?” to “What is this, and how do I solve it?” That is the only question that leads to inner strength and better health.
you may also read nowitstrend.